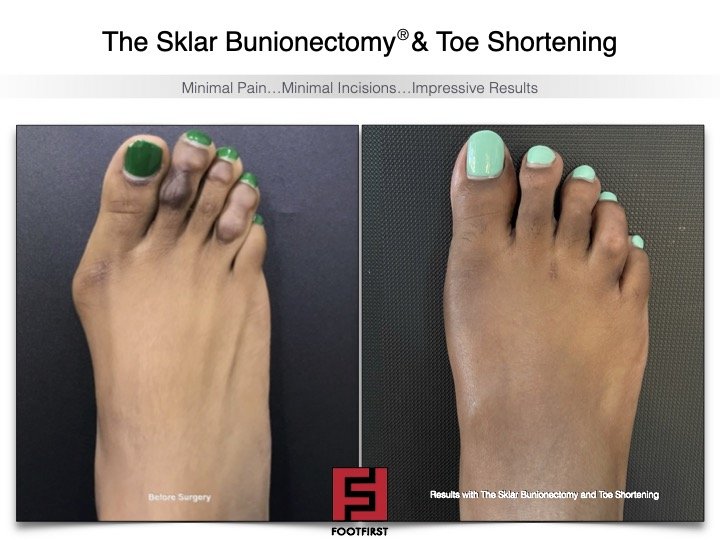
A bunion is a progressive deformity in which the bump on the side of the foot becomes enlarged as the big toe continues to shift or bend in the opposite direction towards the smaller toes. In extreme cases, the big toe will continue to shift until it is sitting on top of the 2nd toe, or more commonly, until it is sitting underneath the 2nd toe. This, in turn, creates another problem as the big toe sitting underneath the 2nd toe can cause a "hammertoe" in which the elevated 2nd toe becomes painful due to pressure and rubbing against the top of a shoe.
A bunion typically becomes painful due to pressure when the bony bump rubs against the side of a shoe. This pressure from the shoe against the skin, nerve, bone, and joint causes redness, swelling, and pain to the bunion area.
Bunions can be seen in both males and females. In our practice, we typically see more females presenting with bunion pain than males because of the type of shoe gear that women wear (i.e. high heels and shoes with narrow toe-boxes). Males also come to the office with bunion pain that is usually caused by ill-fitting shoe gear (i.e. steel-toed work boots or dress shoes with a narrow toe-box). A bunion can be seen in both children and adults. In our office, we have seen child with a bunion that was so severe and painful that surgery was required at 9 years old. It is rare to see a child that young with a bunion so progressed that it becomes symptomatic, but it is much more common than people think to see bunions in the younger population, especially teenagers.
What causes a bunion?
It is more myth than fact that bunions are caused by shoes. Shoes can definitely aggravate and irritate a bunion that has already formed, but the shoes are usually not the cause of the bunion.
A bunion is typically caused by improper foot structure and function. A person is often born with this poor type of foot structure in which the bones are not aligned properly. This improper bone alignment causes faulty biomechanics (the way in which the tendons, ligaments, bones, and joints work together when walking). There is an imbalance in the forces exerted across the big toe joint (1st metatarsophalangeal joint) during walking. The abnormal motion and pressure to the joint leads to joint instability and the tendons begin to the pull the bones (1st metatarsal and big toe) in opposite directions.
We often see many people in one family with bunions (grandmother, mother, aunt, daughter, etc.). This is due to the fact that one can inherit this improper foot structure that is prone to bunion formation.
Other causes of bunions include injury/trauma to the foot or big toe joint area, neuromuscular conditions, osteoarthritis, and inflammatory joint disease such as psoriatic arthritis, rheumatoid arthritis, and gout.
What are possible treatment options for a bunion?
A bunion can be treated both conservatively and surgically. Conservative treatment is always considered the first line of treatment, but it may not be sufficient in certain cases where the bunion deformity and symptoms are so progressed that surgery is the only way to alleviate the pain.
First suggestions to reduce or eliminate bunion pain include wearing shoes that are wider in the toe-box area to accommodate the bunion and reduce pressure and rubbing on the bone. Padding can also be added to the bunion area of a shoe. Cortisone injections to the bunion area can be very helpful because they can greatly reduce the pain, swelling, and inflammation associated with a bunion. Physical therapy and anti-inflammatory medications may be helpful as well.
Another very helpful conservative treatment for a bunion is the use of custom molded arch supports, also known as orthotics. The main reason that a bunion forms is due to faulty or improper foot structure and function. Orthotics can improve the foot function and structure by supporting the foot and holding it in a more proper position. This will reduce the stress on the joints of the foot, especially the big toe joint (1st MPJ), which in turn will reduce the pain. Also with the orthotics properly supporting the foot structure when we walk, they can possibly prevent the bones from further abnormal shifting and keep the bunion deformity from getting larger.
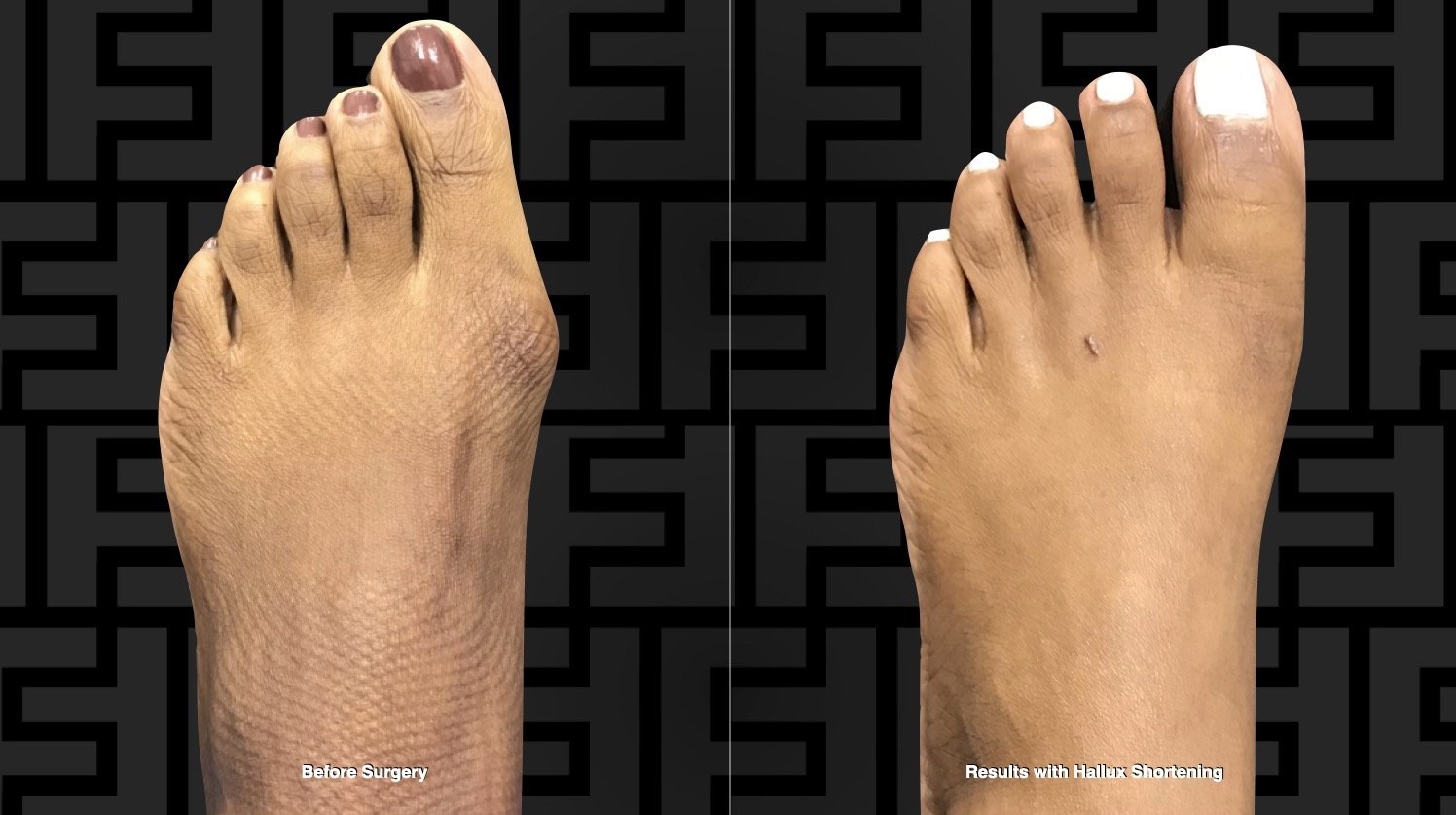
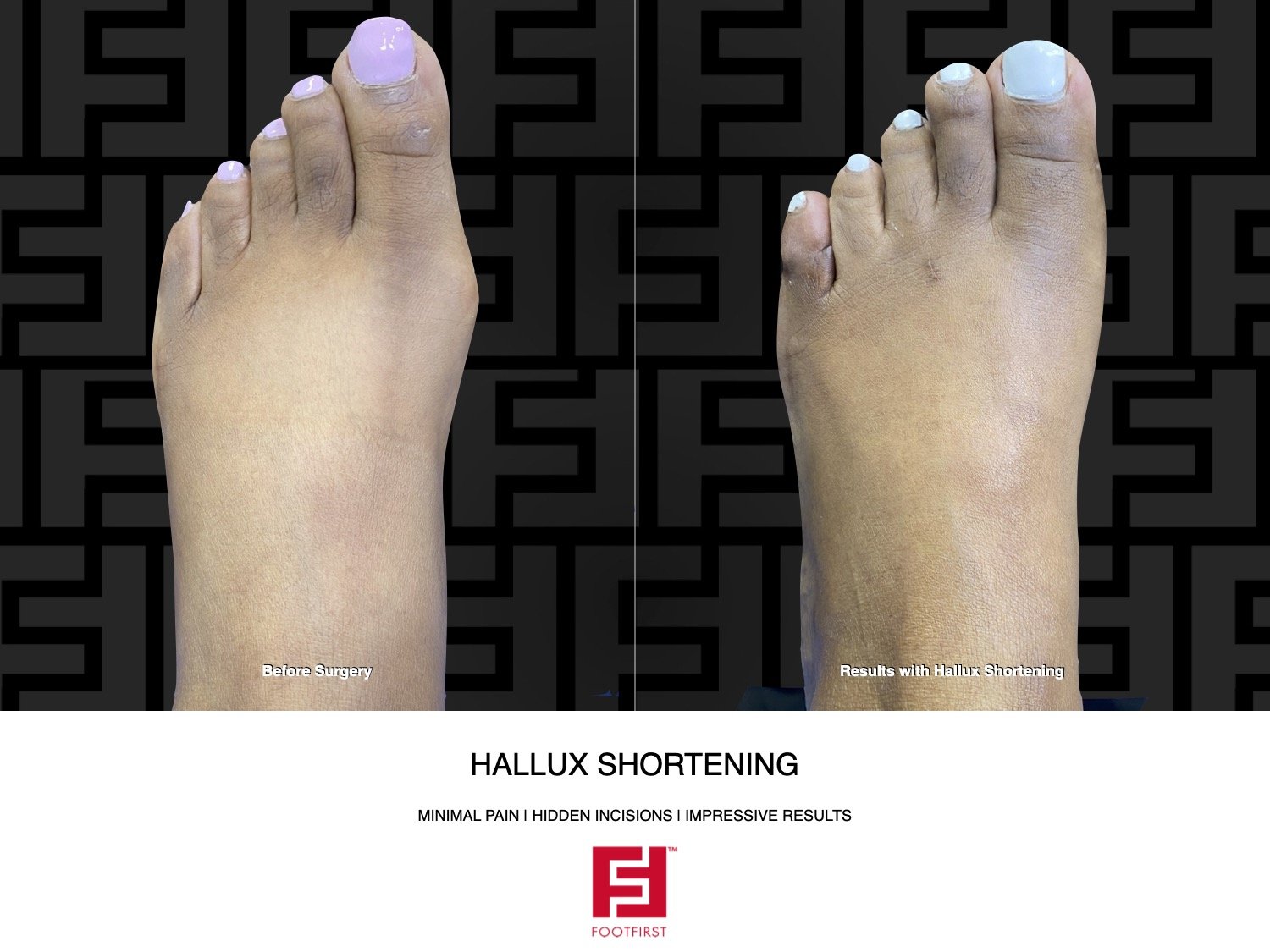
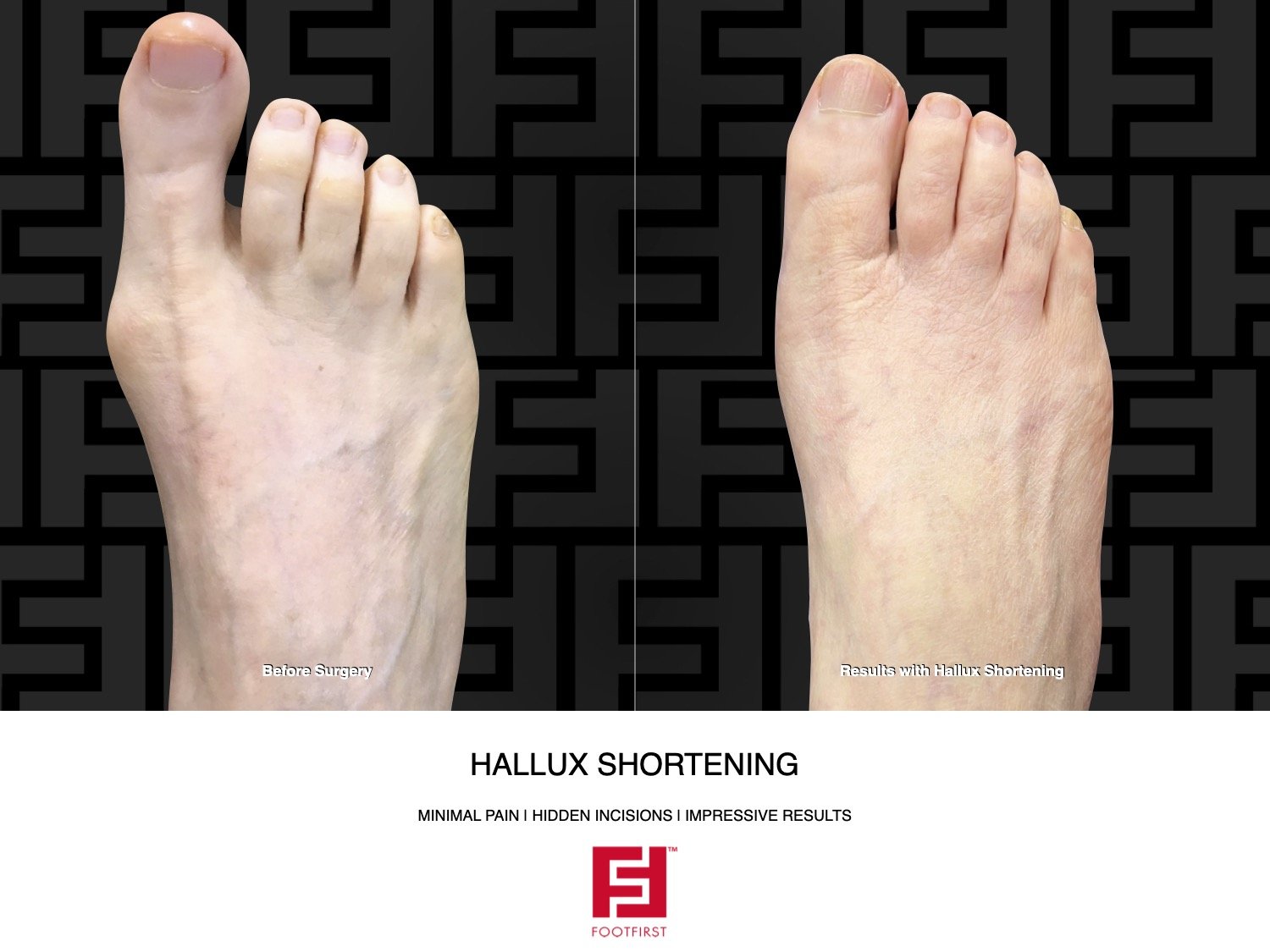
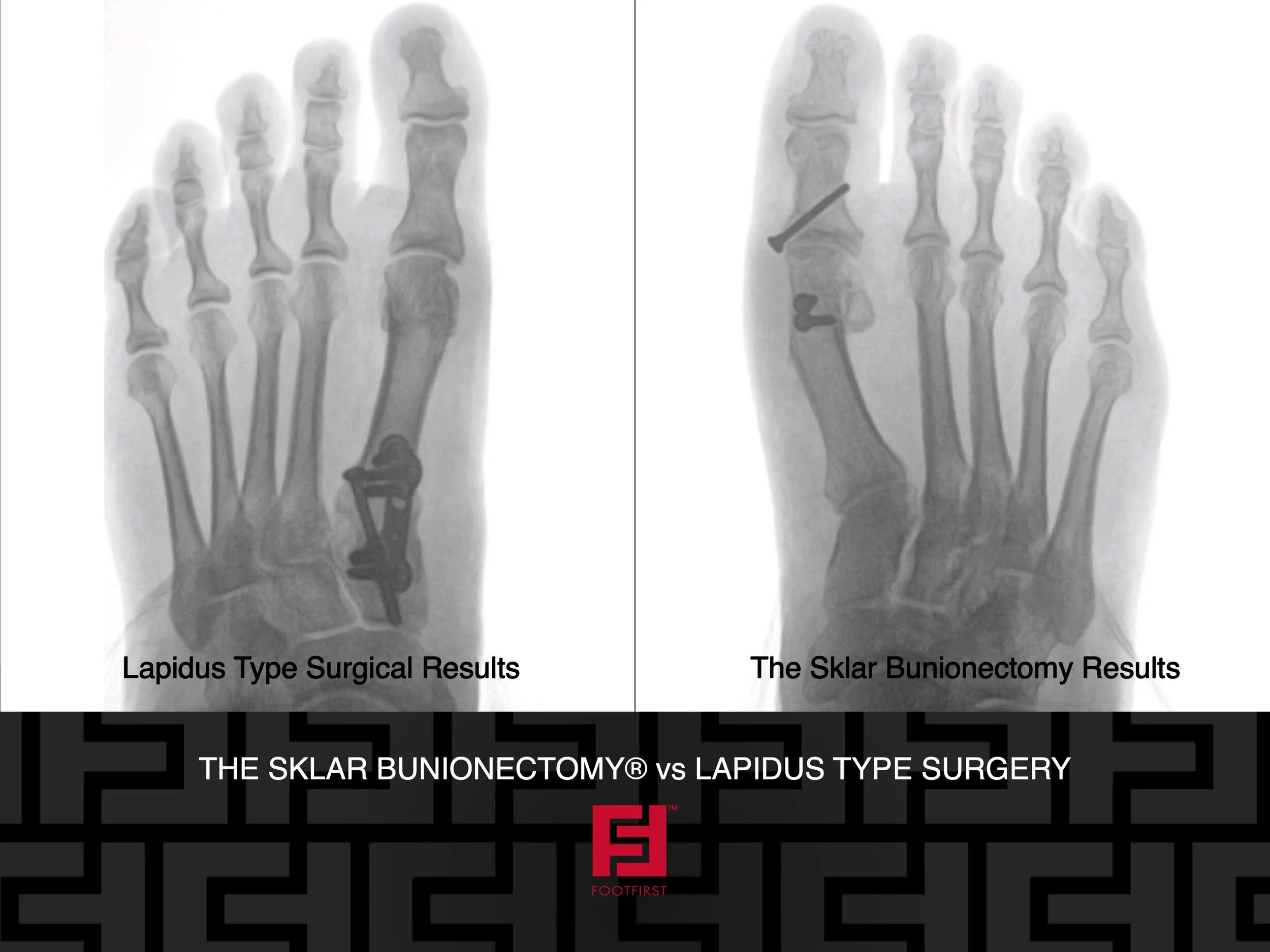
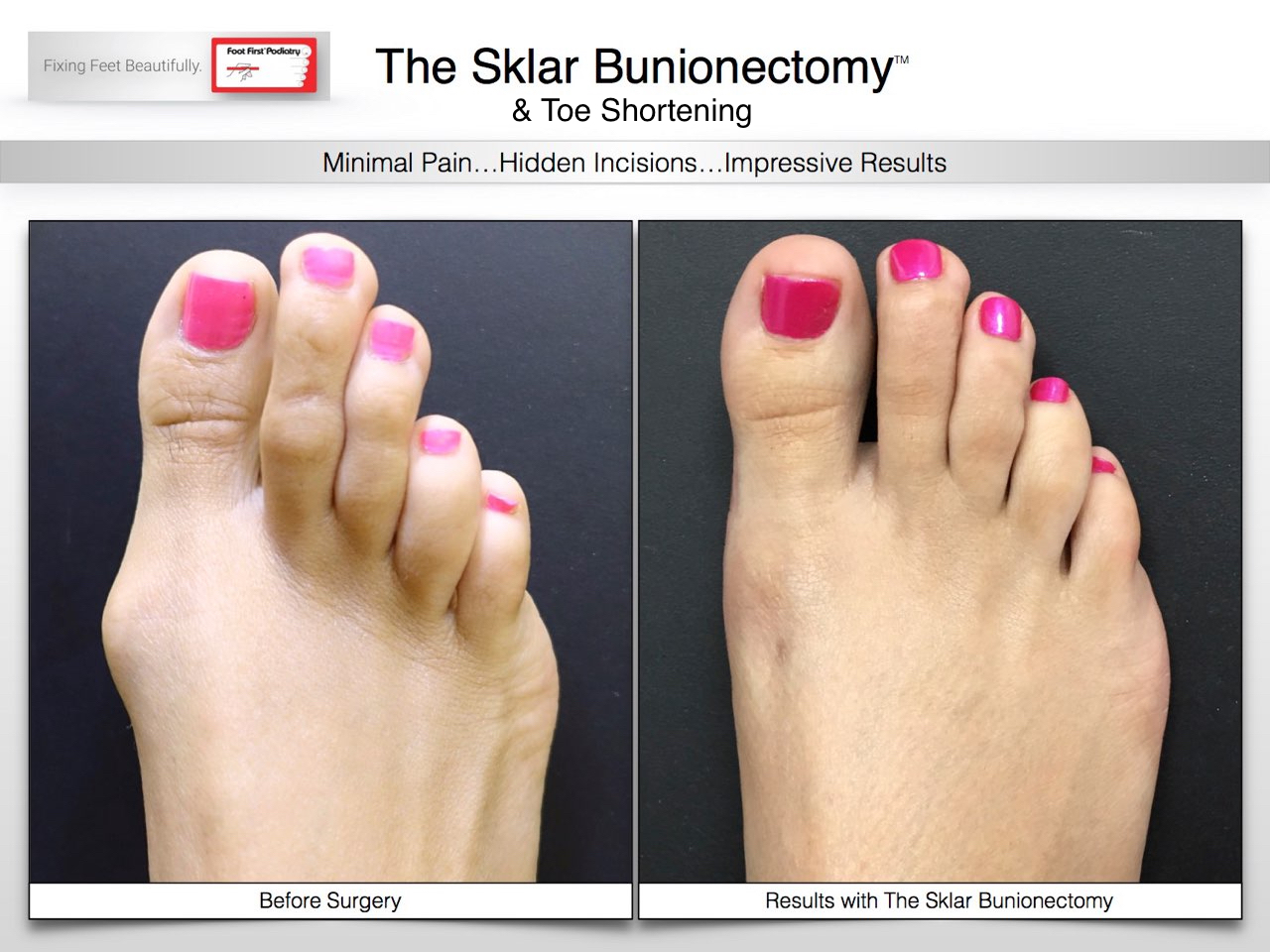
In many cases though, surgery is inevitable. It is the only true way of permanently correcting the root cause for the bunion pain and bunion formation. Surgery is utilized to remove the bunion "bump" and to realign the bones (big toe and 1st metatarsal) that are abnormally shifting and causing the bunion to form. Screw fixation is often used to hold the correction in place after the bones have been "realigned".
Patients are often worried that they will be incapacitated and unable to do anything for months after surgery. In our practice, there are no casts or crutches used and the patient is able to walk immediately after the surgery (with the use of a special surgical shoe). The patient can wear a normal shoe as soon as 2 to 3 weeks after surgery.
Please feel free to call our office at Foot First for a consult regarding your bunion or any other foot and ankle problems you may have. We will gladly evaluate your feet and personally discuss with you all of the possible treatment options that we provide.